Every week, your practice submits claims to insurance companies. Some get paid. Some don't. But do...

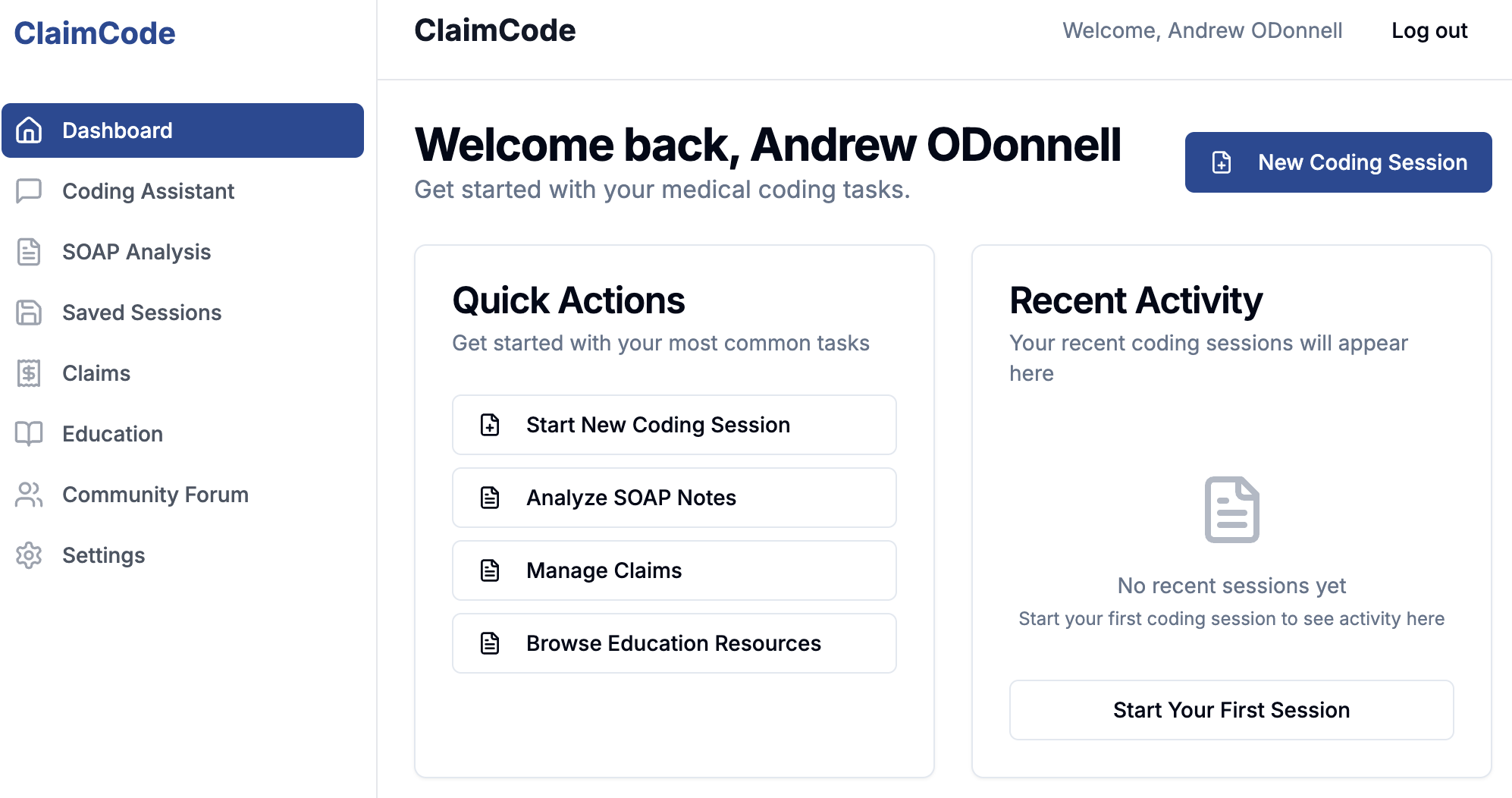
Stop wondering where your revenue is. ClaimCode integrates directly with your clearinghouse to show you every claim's status, every dollar's location, and intelligent suggestions for fixing denials. All in one place.
You submit claims through your clearinghouse. But then what? You're bouncing between your EMR, your clearinghouse portal, and spreadsheets trying to track what got paid, what's still pending, and what got rejected. When a denial comes back, you're manually digging through documents trying to figure out why. It's inefficient and it's expensive.
The industry struggles with this. Denial rates hover around 12-15%, and many practices never even attempt to appeal them. Your revenue is sitting on the table.
Link ClaimCode to Availity, Stedi, or Claim.MD. Your claims data flows in automatically. No need to manual re-enter data. All claims data is read from a single source of truth.
Easily view all of your claims' statuses. Aggregate claim amounts by status, provider, procedure, or diagnosis. See which claims are moving and which need attention.
When a claim is denied or rejected, ClaimCode analyzes the remittance advice and supporting documentation. We explain the reason and suggest exactly how to fix it.
Clearinghouse integration means your claim data comes in once. Your team stops re-entering information across systems.
Every claim on one dashboard. Status, payer, amount, submission date, current location in the pipeline. Know exactly where your revenue is at any moment.
See total revenue that's been paid. See what's still pending. See what's been rejected or denied. Understand your cash flow in real time.
When denials arrive, ClaimCode reads the electronic remittance advice and identifies the root cause. No manual digging through documents.
For every denial or rejection, ClaimCode suggests exactly how to fix it. What modifier to add. What documentation to correct. What payer rule you may have missed.

Your clearinghouse already has all your claims data. Every status update. Every payer response. Every dollar. So why are you logging into three different systems to find out where your money is?
ClaimCode integrates directly with Availity, Stedi, and Claim.MD. We pull your claims data, your remittance advice, and your status updates in real time. Your team gets one unified view. One source of truth. No duplicated data entry. No hunting across platforms.

When a claim is denied or rejected, the acknowledgement or remittance advice comes back with a code (or several). But codes can be cryptic. Payers don't explain themselves.
Your team is left investigating: Was it a coding error? A missing modifier? A documentation issue? A payer-specific rule we missed?
ClaimCode interprets the 277AC or ERA to understand the denial reason. We know your specialty—PT's 8-minute rule, OT's functional limitations, chiropractic frequency limits. We tell your team exactly what is wrong with the claim and how to fix it.
No more phone calls to payers. No more manual document review. Just clear, actionable remediation steps.


It doesn't matter if your a solo practitioner taking on more business or a growing practice ready to open your third location. If your practice is using Availity, Stedi, or Claim.MD, ClaimCode is for you. If you're tired of claims visibility issues and manual denial investigation, we can help solve it.
ClaimCode works for practice owners managing revenue or a team billing administrators handling daily claims work.
ClaimCode gives you the tools to work smarter.

Every week, your practice submits claims to insurance companies. Some get paid. Some don't. But do...

Introduction Starting your own chiropractic or physical-therapy practice is thrilling…until you...

As a physical therapy or chiropractic student—or a recent graduate—managing billing and coding can...